THE OPERATING ROOM
When | Fall 2016
Where | Charleston, South Carolina
Occasion | Clemson A+H Studio Project + AHRQ RIPCHD.OR Grant
Team | Leah Bauch, Kenneth (Qian) Dong, Austin Ferguson, Lindsey Hofstra, Yingce Huang, Max (Shirui) Lin, Jane (Zhiquin) Liu, Rachel Matthews
Other Links | Simulation and Mockup Build Videos, Clemson's Center for Health Facilities Design and Testing Issuu
Brief | This design challenge was sponsored by the Agency for Healthcare Research Quality through a grant for the project Realizing Improved Patient Care Through Human Centered Design in the Operating Room (RIPCHD.OR). This operating room (OR) focuses on ambulatory surgeries in the pediatric and adult orthopedic settings.
At the beginning of the semester the studio was tasked with researching current practices in the operating room, potential products and systems, code analysis and laying out a room data sheet. This document was helpful in informing the team of the possibilities regarding the OR. An initial kick-off of the design challenge occurred with many of the key players on the design and clinical sides at the Charleston Design Center. This afforded the design team an opportunity to express initial thoughts and ideas as well as work with experienced practitioners.
Although the research began in the first year of the grant and continued through to the beginning of the semester, the document was continually refined while the design of the OR evolved. Meanwhile, approximately every three weeks, the design team would assemble in Charleston to conduct simulations with clinical teams from the Medical University of South Carolina. These teams consisted of one ambulatory pediatric team and one adult orthopedic team which included the minimum of four staff members: circulating nurse, scrub nurse, anesthesiologist and surgeon. The simulations ranged from a primitive blue-tape mockup to a full-scale, cardboard mockup. Meeting with and hearing from the clinical team greatly informed the design and was the most rewarding aspect of the design challenge.
DESIGN FRAMEWORK, OBJECTIVES & GUIDELINES
The guidelines were developed throughout the entire semester but was initially begun at the Learning Lab Workshop held at the Cigar Factory in Charleston, South Carolina. This location, also known as the Charleston Design Center, is the current place for the simulations which were conducted throughout the project. It is also, hopefully, the site for the future high fidelity mockup.
These design guidelines serve as a means of informing the design process as well as a future way to evaluate it. Research conducted by the team during the first year of RIPCHD.OR informed the guidelines to bridge the gap between research, design and practice. The overall framework of the process is explained by beginning with the project vision, the design objectives which inform the vision, and the guidelines by which the objectives can be obtained. Each guideline is expanded upon with definitions, when and where it is appropriate, why it is important and the strategies that can be implemented to achieve the guideline.
ROOM & SUITE OPTIONS
Designing a singular room denotes considering the "site" in which the room fits. In surgical suites three types of configurations were explored: clean core, single corridor and the work core. One room configuration fits with the clean core model while the remaining three fit well with the single corridor and the work core. The clean core denotes "sterile" storage within the core model while the remaining three fit well with the single corridor and the work core. The single corridor consists of a double-loaded, two-way traffic corridor. The work core consists of a wider single corridor with two-way traffic and provides ample space for the storage of clean and soiled items (separated). A variety of the room configurations indicate a larger departmental gross square footage than others, therefore emphasizing the importance of its consideration.
O.R. CONFIGURATION OPTIONS
Floor Plan A
Floor Plan A has door locations immediately opposite of one another on the short sides of the OR. The circulating zone connects the two doors making it an optimal place for the circulating nurse to be located. The door on the bottom of the plan is designed to lead to the clean core. There is recessed storage conveniently located in the anesthesia zone and the circulating zone. During simulations with MUSC, staff verbalized the need to have storage located in those zones for immediate access to items needed for every surgery as well as some unique procedures.
Floor Plan B
Floor Plan B consists of Plan A with a singular door which complies with the single corridor and work core. The circulating nurse still maintains access to the exit door in order to retrieve any items stored outside the OR. Plan B also illustrates the possibility of incorporating an adjacent storage room and / or control room. This configuration enables the possibility for the room to expand in the short dimension or incorporate future procedures that may require more imaging equipment and personnel. Plan B also illustrates the possibility of a full window wall at the bottom of the room plan.
Floor Plan C
Floor Plan C is very similar to Plan B yet is rotated 90 degrees counter-clockwise with the door and scrub sink located on the long side of the room. The zones within the room fundamentally do not change but further create flex zones which enable the room to adapt when the procedure takes place on the right or left side of the patient’s body. This plan also features the possibility of a storage and / or control room on the short side of the room. The placement of the window wall alters in this plan and simulations with MUSC staff has informed the design to incorporate windows below displays on the bottom wall.
Floor Plan D
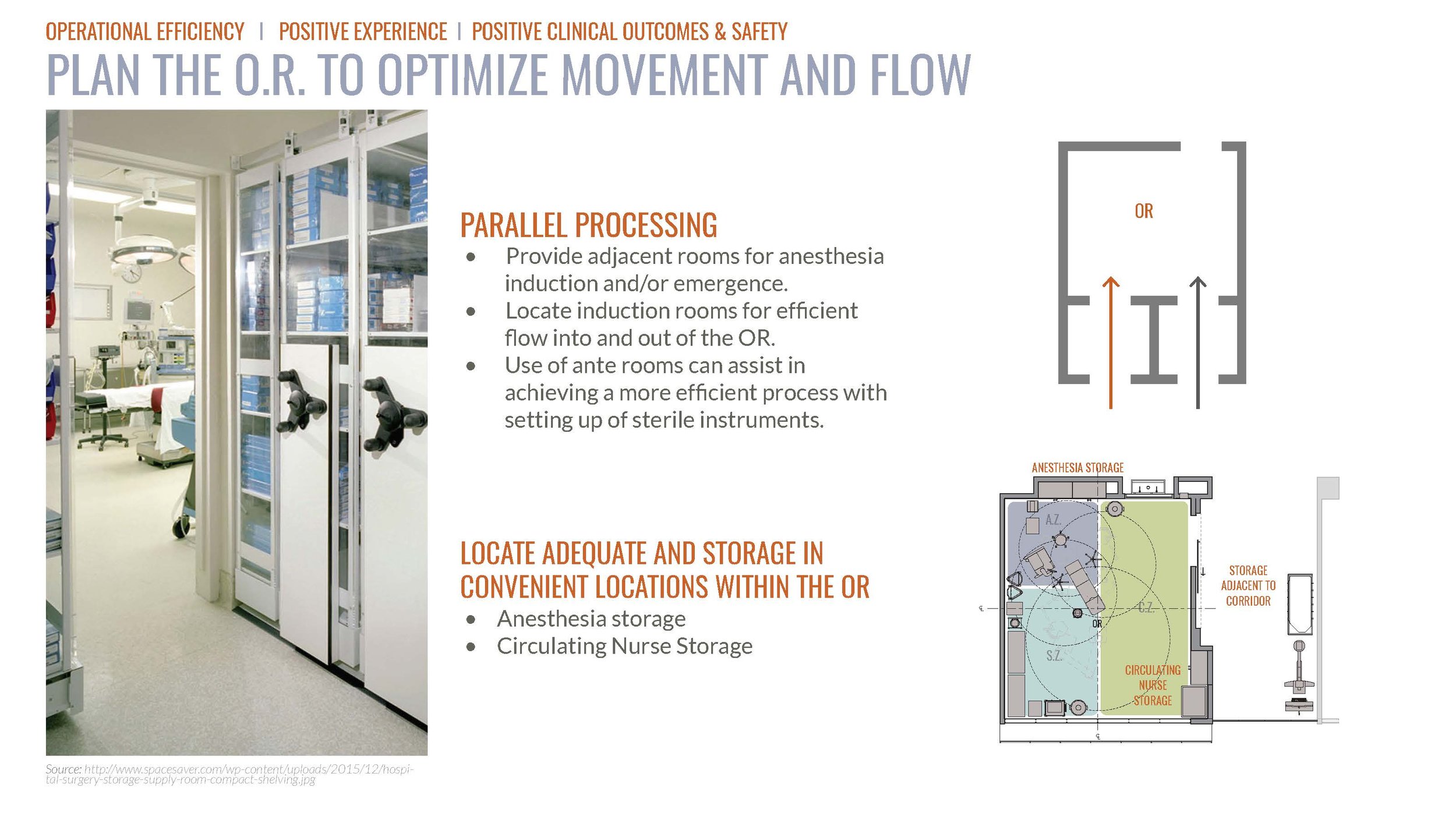
Floor Plan D is the induction room configuration. Through case study analysis and research, the design team indicated the importance of exploring the option of the double induction room model. Plan D has three doors placed on two walls of the OR. This fact alone highly constrains the space yet allows the surgical process move more efficiently when appropriately scheduled and staffed.
SURGICAL PHASES
Patient Preparation
The patient is brought into the OR from pre-op, feet first, on a stretcher by a member of the anesthesia team and may or may not be assisted by the circulating nurse.
The stretcher is then pushed parallel next to the surgical table while the anesthesia team member and circulating nurse aide in transferring the patient onto the table.
The patient is then induced while the scrub nurse / tech prepares the required instruments on the back table.
Intraoperative
Once the patient is induced the team completes “time out” in which the patient is verified again, procedure checked, incision site checked, etc.
The anesthesia team remains relatively stationary during this phase but monitors the patient’s vitals as well as the status of the surgery.
The surgeon / resident are located on either side of the surgical site while the scrub nurse / tech hands each instrument to the surgeon / resident when needed.
The circulating nurse remains attentive to the needs of each person in the room and is prepared to retrieve any items necessary that are not located in the OR. The circulating nurse also charts during the procedure.
Patient Preparation
The surgery concludes and the surgeon / resident closes the surgical site, if present.
The anesthesia team then brings the patient out of induction while the surgeon begins charting.
The scrub nurse / tech begins to count and reorganize all the instruments opened during the case.
The circulating nurse assists anyone needing assistance.
Once the patient is stable the anesthesia team transfers the patient from the surgical table to the stretcher. The anesthesia team them moves the patient to the post-op area.